By Kate Hawkins, Maryse Kok, Kingsley Chikaphupha and Meghan Bruce Kumar
“There is significant data collection through various methods and implementers of community health. HSA’s are technically assigned to complete over 40 M&E forms and processes while there are currently 15 different types of data used in community health. The amount of data collection creates a burden for implementers around consistency and quality of data that is weakened by insufficient quality assessments and training for data collection… Multiple processes for data collection also raises questions around data quality given the amount of time needed to devote to multiple M&E processes as well as limited trainings and supervision.”
Malawi National Community Health Strategy 2017 - 2022
As the drive for Universal Health Coverage and the Sustainable Development Goals (SDGs) has led to a push for greater health service access, the issue of sustaining and embedding quality in the ways in which these services are delivered has gained prominence.
Measurement of quality and attribution of its effects in health is challenging at any level. But little is known about how quality is assessed within community health programmes, who are on the frontline of health service delivery in many low- and middle-income settings. The degree to which new initiatives like the Lancet Commission on Quality in Health Systems will include community health programming and the role of close-to-community health providers is currently unclear.
Health systems are shaped around well analysed power asymmetries. Relatively less powerful staff who labour at the interface of the community and health sector are rarely canvassed on their opinions of quality nor are their voices prominent in the decision-making processes that effect their daily labour. At the more local level differences in the personal characteristics of community health workers and their supervisors (such as sex, educational level, class, experience of poverty etc.) also act to reinforce power asymmetries.
This brief explores how close-to-community health providers in Malawi perceive quality as an aspect of their work and highlights some key challenges which may hinder the definition, measurement, and achievement of quality at the community level. It is based on research conducted by REACH Trust.
We found that Health Surveillance Assistants, the community health workers that operate in Malawi, experienced many challenges which hindered the provision of what they would consider a ‘quality’ service, these included:
- Inadequate training on quality improvement/assurance and a lack of incentives for peers to learn from each other on this issue
- Supervision which was not supportive and which rarely focused on quality of care. Where progress was measured against quality indicators this tended to be partial and limited to a handful of programmes
- That guidelines on topics like task shifting had not reached the district level and below and when they are received they are not always used
- Erratic monitoring visits
- Multiple quality measures that were related to the plethora of vertical interventions which are managed by NGOs in addition to those required by the government
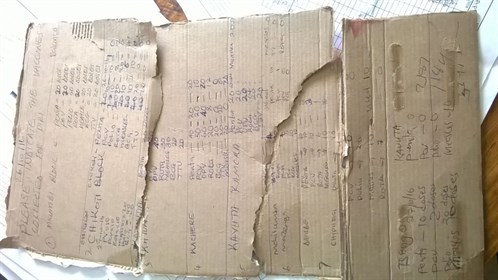
- A lack of standard Ministry tools to enable HSAs to measure progress which leads HSAs to create their own informal summary activity reports which are often supplemented by a multitude of programme-specific reporting forms (e.g. for nutrition, iCCM, family planning).
- A lack of pre-testing of new tools which means that they are not always fit for purpose
- Poor data quality at community level which is reported on an ad hoc basis if/when requested by NGOs or HSAs. When this data is collected it is not always analysed or interpreted. Collated data is not consistently fed back to communities so that they can make changes
Read the brief to find out more.
Latest news
- Do devolved Kenyan county governments prioritise universal health coverage?, 10 August 2017
- Improving maternal health in Shebedino district, Ethiopia: Positive stories need to be told, 1 August 2017
- Universal Health Coverage: The economists’ perspective, 26 July 2017

This project is funded by the European Union.
